Abstract:
Keratoacanthoma is a rapidly evolving tumour of the skin, composed of keratinizing squamous cells originating in the pilosebaceous follicle.[1] It can progress very rarely to squamous cell carcinoma. It affects the sun-exposed area in the sixth or seventh decades. In temperate regions, 70% keratoacanthomas are localized on the face while in the subtropics they involve the arms, dorsa of hands and lower extremities. Surgical excision is a modality of treatment. Overall recurrence rate is 2.4%. [2]
Introduction:
Keratoacanthoma was first described by Sir Jonathan Hutchinson in the 1880s.[3] It affects sun-exposed areas in Fitzpatrick’s skin types 2 and 3. It presents usually as a solitary dome shaped erythematous skin coloured nodule with a central keratin plug. After a rapid initial growth phase, it spontaneously involutes in 4-6 months. Recurrences occur especially when the tumour is present on trauma-prone regions like hands, fingers, lips or ears. There are various variants of keratoacanthoma; out of which giant keratoacanthoma are locally aggressive without metastasis. They are difficult to differentiate clinically and histopathologically from highly differentiated squamous cell carcinoma. In this report, we present a case of giant keratoacanthoma which was treated with surgical excision.
Case Report:
A 56 year-old female patient, farmer by occupation, presented with an asymptomatic rapidly growing tumour on the nose for a year. The swelling started as a nodule which rapidly grew in size with peripheral extension. It further developed raised rolled out margins and a central depression.(Fig 1) The size of the lesion was about 3 cm x 4 cm x 1 cm, located on the bridge of the nose.(Fig 2) It was firm to hard in consistency. There was no bleeding or tenderness on palpation. Differential diagnosis of Cutaneous Leishmaniasis, giant Keratoacanthoma, keratoacanthoma Centrifugum Marginatum and Squamous Cell Carcinoma were considered.

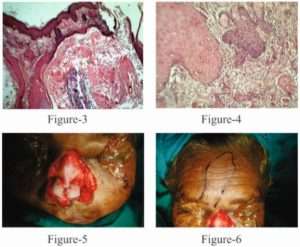
The lesion was surgically excised with a wide margin and wound was closed with flap surgery. (Fig 3, 4, 5)Tissue was sent for histopathology. On histopathological examination after H and E staining, a well circumscribed circular lesion was seen, with a central cup shaped crater which was filled with keratin. (Fig 6) At either side of the lesion, epidermal buttressing was present. A few horn pearls were also seen. (Fig 7) No cells containing LD bodies were seen. Thus, the diagnosis of Keratoacanthoma was confirmed. The patient has regularly consulted us for the last three years, with no evidence of recurrence.
Discussion:
A Keratoacanthoma was described by Freudenthal of Wroclaw in the 1940s.[3] Keratoacanthoma develops with an aggressive and infiltrative nature. Keratoacanthomas larger than 20-30 mm are termed as Giant Keratoacanthomas.[4] Less than 50 cases are reported in literature. It is an acquired disorder with no genetic predisposition. Several factors are involved in the pathogenesis of Keratoacanthoma that includes ultraviolet radiation, smoking, contact with chemical carcinogens like pitch, mineral oil, tar, trauma and vaccination.[5] Giant Keratoacanthoma occurs on the eyelid and nose. Our patient had a lesion on the nose. Being a farmer by occupation, exposure to ultraviolet radiation and trauma could be the probable etiological factors.
Progressive peripheral extension with a raised rolled-out margin and atrophy at the centre is a characteristic feature of Giant Keratoacanthoma which was seen in our case. This sort of typical appearance may arise as a result of sequential involvement of multiple hair follicles in a centrifugal fashion.[6]
Giant Keratoacanthoma causes destruction of underlying tissue and spontaneous involution takes place after several months, often accompanied by detachment of a large keratotic plaque. Keratoacanthoma lesions are benign and regress spontaneously. Locally aggressive nature of Giant Keratoacanthoma creates diagnostic difficulties for the dermatosurgeon as to differentiate from a malignant tumor like Squamous Cell Carcinoma.
Giant Keratoacanthoma has been treated successfully with oral retinoids.[4,7] which should be given until complete clearance of lesion. If surgery is not possible, radiation therapy can be considered. Other treatment modalities successfully used include topical 5- Fluorouracil[9,10], intra-lesional injections of interferon Alpha-2a[4,11], Methotrexate[13], or Bleomycin, or Mohs micrographic surgery.[12]
Surgical intervention should be a preferred mode of therapy as it totally removes the tumor. Being a lesion in an elderly patient on sun-exposed areas and as it was locally aggressive, we opted for wide surgical excision. This achieved the best cosmetic results with minimal scarring.
Conclusion:
Keratoacanthoma is a fast growing aggressive tumor with spontaneous regression. Development of giant variant of Keratoacanthoma with infiltrative and aggressive behavior is known which enables dermatologist to differentiate it from highly differentiated Squamous Cell Carcinoma. Surgical excision like flap surgery is a treatment of choice for Giant Keratoacanthoma.
We are presenting this case for its relative rarity in the Indian scenario and for the good cosmetic results obtained as well as the lack of local recurrence after a number of years of follow-up.
References:
- MacKie RM, Quinn AG. Non-Melanoma skin cancer and other epidermal tumors. In: Burns T, Breathanach S, Cox N, editors. Rook’s textbook of dermatology: 8th Singapore: Fabulous Printers; 2010. p.52.42-44.
- Larson PO. Keratoacanthomas treated with Mohs’ micrographic surgery (chemosurgery). A review of forty-three cases. J Am Acad Dermatol. 1987; 16:1040–1044.
- Sujay khandpur, M.Raman (Authors), IADVL Textbook Of Dermatology,Skin Tumors(chapter 46).Third Edition. (editors) R.G.Valia & Ameet R. Valia. Mumbai Bhalani Publishing House.(1475-1538).
- Schwartz RA. Keratoacanthoma: a clinico-pathologic enigma. Dermatol Surg. 2004; 30(2 Pt 2):326–333.
- Piyush B Borkhatariya, Shweta Gupta, Damodar Bang, Ranjan C Rawal. Case report and review of literature:Correspondence: Keratoacanthoma centrifugum marginatum. Indian Journal of Dermatology. 2007; 52 (4): 204-205.
- Kirkham N. Tumors and cysts of the epidermis. In: Elder DE, editors. Lever’s histopathology of the skin. 10th USA: Lippincott Williams and Wilkins; 2009. p. 791-850.
- Schwartz RA. Keratoacanthoma. J Am Acad Dermatol. 1994; 30(1):1–19.
- Meghana M Phiske, Ganesh Avhad, HR Jerajani. Case Report: Keratoacanthoma centrifugum marginatum at an unusual site. Indian Journal of Dermatology. 2013; 58 (1): 74-76.
- Gray RJ, Medland NB. Topical 5-fluorouracil as primary therapy for keratoacanthoma. Ann Plast Surg. 2000;44(1):82–85.
- Parker CM, Hanke CW. Large keratoacanthomas in difficult locations treated with intralesional 5-fluorouracil. J Am Acad Dermatol. 1986;14: 770–777.
- Grob JJ, Suzini F, Richard MA, et al. Large kerato-acanthomas treated with intralesional interferon alfa-2a. J Am Acad Dermatol. 1993;29: 237–241.
- Shriner DL, McCoy DK, Goldberg DJ, Wagner RF., Jr. Mohs micrographic surgery. J Am Acad Dermatol. 1998;39(1):79–97.
- de Visscher JG, van der Wal KG, Blanken R, Willemse F. Treatment of giant keratoacanthoma of the skin of the lower lip with intralesional methotrexate: a case report. J Oral Maxillofac Surg. 2002;60(1):93–95.
*-*-*