Case Report:
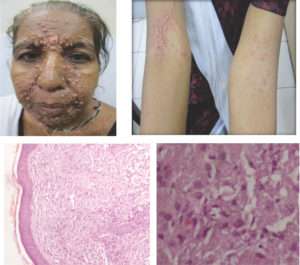
A 40year old housewife presented with the complaints of recurrent episodes of high grade fever from 3 months and asymptomatic skin colored papular eruptions over the central face for last 1 and 1/2 month. Subsequently, the similar papules had appeared over chest, abdomen, back and upper limbs. There was no history of breathlessness, cough, seizures and altered sensorium. Patient was a known diabetic and was on oral hypoglycemic drugs. There was no history of extramarital sexual exposure and blood transfusion. No history of travel beyond nearby locales. Clinical examination revealed that the patient was pale and had hepatospleenomegaly. Multiple skin colored to erythematous discrete as well as coalescing papulonodular lesions ranging in size from 0.2 cm to 1cm present bilateral symmetrically over the central part of the face involving the glabella, medial side of both the eyebrows, nasolabial folds, chin, neck, anterior chest, abdomen, back and both cubital fossa. Few of these papules showed central umblication and central necrosis with haemorrhagic crusts. Oral mucosa was also involved with multiple superficial erosions over hard palate and both buccal mucosa. Patient had generalized lymphadenopathy , lymph nodes were firm, non-tender, mobile, painless with no matting or overlying sinuses. A review of the central nervous system, respiratory system and cardiovascular system revealed no evident abnormality.
Further, the patient was admitted and subjected to a battery of investigations:
- Haematological Studies: Haemoglobin was 8.4 mg%, Total leucocyte count was 8000/μl and platelet count was 2.8 lakhs/μl at the time of admission but these parameters deteriorated with time to Hb- 6 gm%, and TLC- 6000/μl while platelet count was unaltered. The DLC- P73L26E1. On peripheral blood smear the RBCs were normocytic normochromic with few macrocytic normochromic cells, WBCs shows normal morphology while platelet count were adequate. Her corrected reticulocyte count was 1.5%. Her absolute lymphocyte count was 700/μl and CD4 T helper cell count was 289/μl and CD4/CD8 ratio was 1.8.
- Biochemical Investigations: Her random blood sugar was 244 mg%. On LFT, Serum bilirubin (Total)- 2.9mg% while bilirubin(Direct)- 0.9mg%, SGOT levels were 231U/l, SGPT- 6 U/l and Alkaline phosphatase levels were 1460U/l. The total protein levels were 6.2 gm%, serum albumin – 2.5gm% and serum globulin of 3.7 gm%. Her Na+ levels were 138 meq/l and K+ levels were 4.2 meq/l at the time of admission but on treatment with Amphotericin her K+ levels were reduced to 2.8 meq/l. Her HIV status was negative for both HIV 1 and 2. The KFT, Urine routine microscopy, coagulation profile was within normal limits.
- Radiological Investigation: On USG abdomen her liver was 17.8cm with grade II fatty changes while her spleen was 4.3cm with no free fluid in chest and abdominal cavity at the time of admission. The plain chest Xray PA view showed bilateral nodular opacities. The NCCT head showed bilateral periventricular white matter and centrum semiovalehypodensities suggestive of ?Ischaemia ??Infection while rest of the brain was normal.
- Histopathology: The skin biopsy from the papular lesion showed thinned and flattened epidermis. The dermis shows sheets of foamy macrophages containing numerous basophilic dot like inclusion surrounded by a clear halo. The PAS positive bodies were present. All these findings were highly suggestive of cutaneous histoplasmosis.
- Tissue Culture: On Sabouraud’s dextrose agar showed colonies ofHistoplasma capsulatum
- Bone marrow biopsy: The spaces were occupied by cellular bone marrow which comprised of myeloid and erythroid series cells. Adequate megakaryocytes seen showing normal morphology. Histiocytes are seen showing intracellular round to oval structures and these were PAS positive. The above findings suggestive of histoplasma infection involving bone marrow.
Treatment:
Thus, a disseminated histoplasma infection was confirmed and patient was admitted started on I/V Amphotericin infusions(0.5- 1 mg/kg/d) given over 2hrs daily for 7 days. However, patient developed pedal edema and swelling of her body alongwith high grade fever, breathlessness and altered sensorium after 1 week of therapy and and unfortunately succumbed to her disease within 10 days after presentation. Meanwhile, the underlying immunosupressed status except for diabetic status could not be ascertained.
Discussion:
Histoplasmosis, a systemic mycosis caused by the dimorphic fungus Histoplasma capsulatum var capsulatum and Histoplasma capsulatum var duboisii is endemic to many parts of the world. The clinical manifestations range from acute or chronic pulmonary infection to a progressive disseminated disease. After initial exposure to the fungus, the infection is self-limited and restricted to the lungs in 99% of healthy individuals. The remaining 1%, however, progress to either disseminated or chronic disease involving the lungs, liver, spleen, lymph nodes, bone marrow or rarely, the skin and mucous membranes. Most patients who develop disseminated histoplasmosis are immunosuppressed (eg, AIDS, solid organ transplantation, treatment with tumor necrosis factor-alpha inhibitors) or are at the extremes of age. Male gender, smoking, alcoholism, prolonged permanence in a rural environment, with exposure to bats in caves (revealing the occupational risk involved in agricultural and animal husbandry activities), houses, and holes dug in the ground are risk factors commonly found in patients with the chronic pulmonary and subacute/chronic disseminated forms of histoplasmosis. Acute disease is usually a localised pulmonary infection, more common in children after acute exposure to the excrements of birds and cattle. Such patients achieve clinical cure spontaneously, but 58.9% require antifungals. In patients with localised disease or with some dissemianation, Itraconazole is considered as highly effective while in disseminated form Amphoterecin b is recommended.
Despite various investigation, no evidence of underlying immunosuppression was found in our patient.
References:
- Faiolla Rivian Christina Lopes, Coelho Mariana Correa, Santana Rodrigo de Carvalho, Martinez Roberto. Histoplasmosis in immunocompetent individuals living in an endemic area in the Brazilian Southeast. Rev. Soc. Bras. Med. Trop. [serial on the Internet]. 2013 Aug [cited 2014 Nov 21] ; 46( 4 ): 461-465. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0037-86822013000400461&lng=en. http://dx.doi.org/10.1590/0037-8682-0124-2013.
- Etxeberria-Lekuona D, Hurtado Ilzarbe G, Méndez-López I, Pérez Ricarte S, Acha Arrieta V. Acute progressive disseminated histoplasmosis in a young immunocompetent patient. Rev Clin Esp 2013;213(9):95-6.
- Sharma S, Kumari N, Ghosh P, Aggarwal A. Disseminated histoplasmosis in an immunocompetent individual-a case report.Indian J Pathol Microbiol2005;48:204–6.
- Alcure ML, Di Hipólito Júnior O, Almeida OP, Bonilha H, Lopes MA. Oral histoplasmosis in an HIV-negative patient.Oral Surg Oral Med Oral Pathol Oral Radiol Endod2006;101:33–6.