SKIN – The largest organ of the body accounts for approximate 16% of total body weight.
It is not merely an inert body coverage, but it fulfils several important functions such as defensive, thermoregulatory, excretory, metabolite and sensory. Healthy skin is necessary to provide protection against the physical, chemical and biological environmental factors.
The major function of the skin is to maintain homeostasis by preventing uncontrolled loss of water, ions and serum proteins from the organism into the environment. Apart from maintaining homeostasis skin also has some other important functions which include protection from the harmful ultraviolet (UV) light via the pigment system, prevention from microbial infection and it also plays important role in immunologic function.
Epidermis which is the outer most and superficial layer of skin proves to be a critical barrier in providing protection. Barrier in general is defined as an object which separates two distinct spaces and/or prevents the free passage between the two environments.
STRATUM CORNEUM (SC) provides a vital barrier which accounts for over 90% of the barrier function of skin. For the first time, in the 20th Century, Marchionini and Schade applied scientific evidence for the protective function of the water lipid mantle of the skin and introduced the concept of the skin barrier. The skin barrier ensures the integrity of the body and controls the exchange of substances with the environment.
The barrier function of the skin is not fully competent immediately after the birth and develops in the early stages of neonatal period.
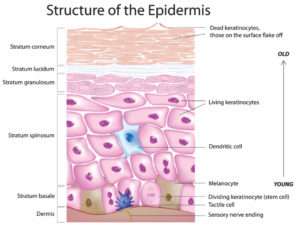
SC made up of flattened, enucleate keratinocytes and compacted keratin granules provides significant protection to skin. This layer greatly varies in thickness depending upon the anatomical area. It is usually 12 to 16 cell layers thick, but it can vary from 9 cell layers thick on the forehead or eyelids to 25 cell layers thick on dorsum of the hand and up to 50 or even more cell layers thick on the palms and soles.
The currently accepted model of the SC as a barrier is a two compartment model in which the protein rich cells, which are the corneocytes are embedded in a continuous lipid rich matrix. Keratohyalin which is a histamine rich protein and the fibrous proteins of keratin are both synthesized within the keratinocytes. Precursors Involucrin and keratohyalin form an envelope around each corneocyte by cross linking, which in turn forms an insoluble exoskeleton which acts as a rigid scaffold for internal keratin filaments.
Characteristics of the barrier :
1. Keratinocytes which are attached to each other through hemidesmosomes provide mechanical strength to the epidermis and are also associated to cytoskeleton proteins.
2. The chemical barrier for the epidermis is through the presence of highly organized acids, hydrolytic enzymes, lipids and antimicrobial peptides.
3. The immunological function of the SC is through humoral and cellular constituents of immune system.
4. There are various mechanisms taking place at the SC which prevents the growth of micro organisms such as the water content drops towards the surface of SC creating hostile conditions for the pathogens. It has an acidic pH and presence of non-pathogenic micro organism on the surface of epidermis also helps to protect against the pathogenic organisms by limiting food availability and by chemical secretions.
Topical drug application has significant advantages over systemic therapy in treating skin diseases due to the ability to directly target the affected skin. Topical application also reduces possible side effects, toxicities, and drug degradation that are commonly seen with hepatic metabolism and systemic drug circulation. Despite the advantages of topical medication, the skin’s barrier function still limits the application of most medications. The kinetics of topical drug delivery is dependent upon the laws of diffusion. Drugs penetrate into the skin through two routes: The transepidermal penetration through intercellular and intracellular pathways, and the transappendageal penetration of sweat glands and hair follicles. Using either route, it is at the SC layer where resistance to drug diffusion is at its highest and has generated interest by researchers to discover new methods of increasing cutaneous drug penetration. One new method being studied to enhance drug delivery is using the combination of topical medications and cutaneous resurfacing.
The relevance of the barrier function to any aesthetic procedure is that they disrupt it and the regeneration process makes the desired outcome. This article discusses about Chemical peeling, Microdermabrasion and Cutaneous Laser Resurfacing and their relevance to the epidermal barrier function.
CHEMICAL PEELING
Chemoexfoliant agents to rejuvenate the skin have been used by people since days of ancient Egypt. Chemical peeling is a method of application of various chemical agents of varying concentrations which cause damage to the skin in a controlled manner.

Peels can be sub-divided on the basis of their penetration into the skin into very superficial peels, superficial peels and deep peels.
Very superficial peels – Remove the Stratum Corneum.
Superficial peels – Penetrate up to Papillary Dermis.
Deep peels – Penetrate up to Reticular Dermis.
Limiting factor of deep peel is high chances of the post procedure pigmentation, particularly in darker skin types, while repetitive peeling sessions are required in superficial peels to get better results.
All peeling agents are assumed to induce three stages of tissue replacement, namely
– Destruction
– Elimination
– Regeneration
All these 3 stages are accompanied by a stage of controlled inflammation.
Controlled partial thickness injury is produced by chemical peeling. Following chemical peeling, a wound healing process ensues which regenerates new epidermis from the surrounding epithelium and adnexal structures that leads to the development of new dermal connective tissue.
The healing process involves the following stages:
– Coagulation
– Inflammation
– Re-epithelialization
– Granulation tissue formation
– Angiogenesis
– A prolonged period of collagen re-modeling.
The continuous clinical improvement in the skin which is seen in the following months after the peel procedure is because of this prolonged period of collagen remodeling. The result is an improved clinical appearance of the skin, with fewer rhytids and decreased pigmentary dyschromia.
The effectiveness of a given peeling agent depends on its concentration and pH.
MICRODERMABRASION
Microdermabrasion is a treatment that uses spray of micro crystals in order to remove the outermost layer of skin cells and thereby revealing

healthier-looking skin. Microdermabrasion treated skin showed gross and histologic improvement which was reported in 1985 by Marini and Lo Brutto of Italy.
Clinically, it is the mechanical exfoliation procedure for superficial skin resurfacing.
Microdermabrasion involves:
– Use of closed loop
– Negative pressure system of debriding Aluminum oxide crystals in order to ablate the superficial layers of the epidermis.
Aluminum oxide is the preferred choice because of its inertness, superior abrasion qualities compared to others and hardness.
Microdermabrasion is technically easy to use. The hand piece consists of a vacuum that draws the skin in when passed over the area to be treated. The depth of abrasion depends on three factors:
– Speed of the pass
– Pressure of crystals being propulsed
– Pressure on the hand piece
For most of the Microdermabrasion treatment the target depth is the removal of Stratum Corneum, but, it can vary from superficial thinning of SC till the penetration to the upper papillary dermis.Repetitive intra dermal injury can result in gradual improvement of the photo damaged skin by stimulating the activity of fibroblasts and deposition of new collagen in the dermis. This can be achieved by repetitive sessions of Microdermabrasion which helps in maintaining the epidermopoiesis. Microdermabrasion is often considered as the basic skin treatment which any individual of any age can undergo.
Microdermabrasion also helps for the enhanced drug delivery of topical drugs. Microdermabrasion results in an increased production of a wide variety of compounds associated with wound healing and skin remodeling like cytokeratin 16, antimicrobial peptides, matrix metalloproteinases, and collagen precursors. Skin barrier changes post microdermabrasion shows changes in TEWL, hydration, and erythema. There is significant increase in TEWL immediately after and at 24 hours after the procedure which returns to baseline 24 hours post-treatment. Overall, the skin barrier function recovers within 48 hours of microdermabrasion.
CUTANEOUS LASER RESURFACING
Cutaneous laser resurfacing has dramatic and reproducible improvement on appearance of photo aged skin. The overall improvement in the skin is achieved as a result of reduced solar-induced dyspigmentation. The two principle lasers used for this are CO2 fractional laser and Er: YAG laser. And both work on a similar mechanism by ablation of photo damaged skin, contraction of thermal collagen and stimulate immediate and delayed collagen remodelling. When tissue is heated to its boiling point, tissue ablation occurs.
Cutaneous laser resurfacing revolutionized after the concept of fractional photo thermolysis. Fractional photo thermolysis works on the principle

of creating full thickness columns of thermal injury (MTZs or Microthermal Treatment Zones) in a pixilated manner leaving the surrounding skin intact below the level of SC. Healing is rapid without crusting or oozing because epidermal barrier function remains intact. In order to get a better skin texture and stimulate the formation of new collagen patients often require multiple sessions in series.
The photothermolysis by Ablative Fractional Lasers (AFL) allows vertical column arrays of MTZs to extend beyond the Stratum Corneum. It is this laser microporation that allows greater drug diffusion and delivery through these newly formed channels to areas beyond and surrounding the Stratum Corneum. The depth and width of the micropores can be modulated to control the rate of drug delivery into the skin. As additional topical medications are recognized as potential combination therapy candidates, more clinical and aesthetic applications for laser assisted drug delivery are being uncovered.
CONCLUSION
The development of technological advancements regarding the barrier function of the skin and new treatment methodologies within skin resurfacing has brought about several emerging therapies. Many of these new therapies demonstrate promising results that closely approach the efficacy of the ablative technologies in clinical outcomes, while further minimizing downtime and side effects. As the demand continues to grow, more research is needed to develop the next innovative resurfacing treatments that continue to improve upon efficacy and safety.