Successful and Safe use of “SCALP THREADING” using PDO Threads in Male Androgenetic Alopecia
Disclaimer: A part of this study has already been accepted for publication in the Journal of European Academy of Dermatology & Venereology, vide (MS no. – JEADV-2017-0505.R1)
Bharti S, Sonthalia S, Patil P, Dhurat R. Scalp threading with polydioxanone monofilament threads: A novel, effective and safe modality for hair restoration. J Eur Acad Dermatol Venereol [In Press]
INTRODUCTION
Androgenetic alopecia (AGA) results in significant disturbance in self-perception and psychosocial interaction in both genders. Although various treatment modalities including topical minoxidil (MNX), oral finasteride (FIN), synthetic bio-peptides, platelet rich plasma (PRP) and many others have been used with good therapeutic benefit, they either show suboptimal response or the response tends to plateau off with no further gain in hair regrowth.1 Hair transplantation is often not a acceptable to many patients owing to it being a surgical modality and/or the cost involved.
Polydioxanone (PDO) threads have emerged as a popular procedure for non-surgical face lift. Multiple modes of action have been suggested and confirmed histologically, including a foreign body reaction-induced neocollagenosis, mechano-transduction which is the fibroblastic response such as actin polymerization and matrix deformation in response to mechanical stimuli, and finally regulation of gene expression, cell differentiation, microcirculation stimulation, and promotion of tissue growth.2
Microneedling using a dermaroller, is another efficacious facial rejuvenation procedure that creates micropunctures leading to a wound healing cascade with release of various growth factors such as platelet derived growth factor (PGF), transforming growth factor alpha and beta (TGF-α and TGF-β), connective tissue activating protein, connective tissue growth factor, and fibroblast growth factor (FGF).3,4 This effect has been extrapolated to stimulate hair growth, confirmed by the results of a randomized double blind trial.4 Akin to the extension of microneedling from facial rejuvenation to stimulation of hair growth procedure, we attempted to assess the response to the insertion of PDO threads into the scalps of 5 male patients with Grade 3-4 AGA, and evaluated the role of this technique as a therapeutic modality for AGA.
PATIENT SELECTION
Based on the above premise, we evaluated the efficacy & safety of PDO thread insertion into the scalp in five male patients of AGA not responding satisfactorily even after 18 months of therapy with both MNX (10% lotion twice-a-day) and oral FIN (1 mg daily). A detailed patient counseling was done regarding the procedure, expectation of results, post-procedure care and expected time of any appreciable response (at least 6 months after the procedure), and written consent was taken. All patients were already off from both the treatments, i.e. oral FIN, and topical MNX, for at least 3 months prior to enrolment for the PDO threads insertion, and they were advised to maintain abstinence. The procedure was undertaken after ruling out diabetes and infections including HIV, Hepatitis B, hepatitis C, and syphilis. None of the patients had any significant systemic or metabolic disorder, keloidal tendency or on anti-platelet or any other drugs. In all patients, hair loss and recession were confirmed to be of AGA origin by detailed history, physical examination and trichoscopic analysis. The hair pull test was performed to rule out active effluvium.
EFFICACY EVALUATION
Global pictures of the frontal scalp, vertex, lateral and back view were taken before and after the procedure for comparison. After baseline global photographs, the scalp were shaved off to ensure equal length of hair shaft in all. Hair count was done trichoscopically in 1 cm2 targeted fixed area at baseline and at end of therapy (week 12). The primary end-point of improvement evaluation was the global photographic improvement (GPI), with secondary end-points being: 1) comparison of the trichoscopic hair count in the target area, and 2) degree of patient satisfaction on visual analogue score (VAS) ranging from 1-10.
METHODOLOGY: Thread Insertion
After signed consent, topical anaesthetic cream was applied over the treatment area 1 hour prior to the procedure, following which the treatment area was thoroughly cleansed with spirit and povidone-iodine. Monofilament PDO threads (30 mm long) were then inserted in the intrademal plane, extending from a pre-decided entry point covering the maximum possible length per needle. Multiple needles were inserted at 1 cm spacing (Fig. 1) in a radial orientation to cover the affected scalp (Fig. 2). The total number of needles inserted per scalp depended on the extent of bald area to be treated ranging from 20-40. During insertion, the scalp skin was stretched by the surgeon’s non-dominant hand to make it taut, and the needle was inserted through the desired point by the dominant hand, ensuring that the needle remains as parallel to the plane of the scalp skin as possible. After insertion, the needles were withdrawn leaving the PDO threads in situ.
The patients were recommended oral antibiotics for 5 days, and suggested to use a mild shampoo after 48-hours. They were also cautioned against applying any other topical over the scalp. Follow-up visits were done at 2 weeks, 6 weeks and 12 weeks after the procedure.

Figure 1: Insertion of the polydioxanone-loaded needles at regular spacing into the intradermal plane of the scalp skin.
Figure 2: Around 12-15 polydioxanone-loaded needles inserted into the entire affected scalp area in a radial distribution
RESULTS
Efficacy (Figs. 3 and 4)
There was no appreciable improvement till 6 weeks post-procedure. However, at 12 weeks, all patients (n=5) had variable but appreciable degree of increase in hair counts, with decent coverage of the previously bald areas. Global photography improvement (investigator evaluated) was significant in all patients resulting in 40-75 % with an average of 57%. The increment in the count of hair follicular units (HFU) by trichoscopy was observed in all patients. Hair count increased from average number of 48 HFU/cm2 to 93 HFU/cm2, with an average gain of 67 HFU per cm2. The patient satisfaction was good with VAS ranging from 4-8 with a mean of 6. The detailed results are mentioned in Table 1. Incidentally, the best outcome was observed in the youngest patient and the oldest patient in our series had the least improvement amongst the group.
Table 1. The results of scalp threading in 5 male patients with androgenetic alopecia at 12 weeks
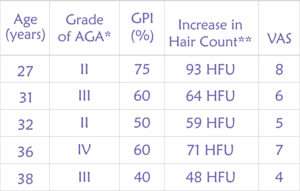
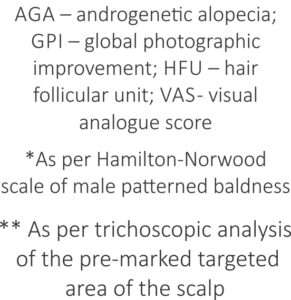
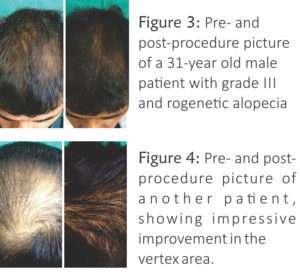
Figure 3: Pre- and post-procedure picture of a 31-year old male patient with grade III androgenetic alopecia
Figure 4: Pre- and post-procedure picture of another patient, showing impressive improvement in the vertex area.
Adverse effects
The procedure was very well tolerated by all the patients with the most common complaint being mild pain during thread insertion (n=5), followed by mild transient swelling (n=2) that resolved within 24 hours. There was no case of significant bleeding, ecchymosis, persistent pain, headache, or post-procedure infection. There were no other adverse effects till the last follow-up.
DISCUSSION
Polydioxanone (PDO) filament is a synthetic absorbable suture which is prepared from polyester, poly (p-dioxanone). It has high flexibility, high retention strength, non-allergenic and a slow absorption rate (6-8 months). It carries no risk of bacterial colonization or infection. When used for non-surgical face lift, threads stimulate neocollagenosis within 2-3 weeks with clinical results expected to last for 2-3 years.1 Although these threads are also available as barbed and screwed, we preferred monofilament threads.
The exact mechanism of action of hair growth stimulation by PDO threads remains speculative. However, it is likely that it is similar to that of microneedling, probably involving enhanced expression of hair-related genes, and release of growth factors like PDGF, and possibly, direct activation of stem cells in the hair bulge area.3,5 A recent randomized evaluator blinded trial by Dhurat et al. had indeed displayed the superiority of the combination of microneedling with MNX versus MNX alone in MPHL (grade III vertex or IV) patients.4
Although this pilot study seems to offer scalp threading as a novel efficacious and safe non-surgical approach to hair regrowth, further research with a properly designed controlled trial with a larger cohort is warranted to elucidate its role in the therapeutic armamentarium of hair restoration. The limitations of this study include the small number of cases, limited duration of follow-up period, and lack of histological analysis of the scalp skin post-thread insertion. Further, unlike the predictable time span of the effect of threads in facial rejuvenation, the duration of the hair growth stimulating effect of the threads remains to be explored. Also, one needs to be cautious about the development of foreign body granuloma in any PDO inserted patient.
References
- Sonthalia S, Daulatabad D, Tosti A. Hair Restoration in Androgenetic Alopecia: Looking Beyond Minoxidil, Finasteride and Hair Transplantation. J Cosmo Trichol 2016;2:1-13.
- Suh DH, Jang HW, Lee SJ, et al. Outcomes of polydioxanone knotless thread lifting for facial rejuvenation. Dermatol Surg 2015;41:720-5.
- Jeong K, Lee YJ, Kim JE, et al. Repeated microneedle stimulation induce the enhanced expression of hair-growth-related genes.Int J Trichology 2012;4:117.
- Dhurat R, Sukesh M, Avhad G, et al. A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: a pilot study. Int J Trichology 2013;5:6-11.
- Kim BJ, Lim YY, Kim HM, et al. Hair follicle regeneration in mice after wounding by microneedle roller.Int J Trichology 2012;4:117.






