Introduction:-
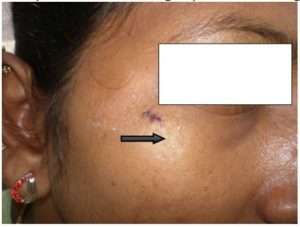
Melanocytic naevi are common benign skin conditions in Dermatology. Majority of the lesions usually go un-attended unless it causes aesthetic concerns or becomes symptomatic. Proper management of the naevi offers both the patient and the treating physician a high degree of result oriented satisfaction.
Definition:-
Naevi means “birthmark” or “maternal impression”. They are benign clusters of melanocytic naevus cells arising due to proliferation of melanocytes at the epidermis, dermal–epidermal Junction or the dermis.
Etiology:-
Melanocytes are pigment producing cells of the body. Their major function is to produce melanin. Melanocytic naevi are derived form melanoblast cells which are in turn derived from the neural crest cells during embryogenesis. Some of these melanocytes complete their migration towards the basal layer and dermo-epidermal junction while some get arrested in the dermal region. Melanocytes may be found distributed throughout the dermis, around and within the walls of blood vessels, around adnexal structures such as hair follicles, within the subcutaneous tissue and sometimes within skeletal muscle, smooth muscle bundles, nerves, or sebaceous glands. These various locations of melanocytes results in varied types of melanocytic naevi.
Clinical Features:-
Naevi are common cutaneous findings and appear on almost all human skin. They are found to be less frequent at birth and increase in incidence during the first 3 decades of life. Various studies suggest that the number of acquired melanocytic naevi is a factor dependent on genetics and sun exposure. Melanocytic naevi are essentially classified as:-
- Congenital melanocytic naevi
- Acquired melanocytic naevi
Dermatosurgeons commonly encounter the acquired type of melanocytic naevi for excision or removal usually for aesthetic purposes. The acquired nevi are benign proliferations of melanocytic naevus cells which are biologically stable and develop from birth. However, melanocytic nevi can be found in association with melanoma. The true frequency of transformation of a melanocytic nevus into melanoma is not known and the estimated prevalence varies, with some data suggesting that up to 40% of melanomas are associated with a precursor melanocytic nevus. According to one study the single greatest predictor of risk for developing melanoma is the total number of nevi.
Classification of Acquired Melanocytic Naevi:-
Common acquired melanocytic nevi are generally less than 1 cm in diameter and evenly pigmented. Some atypical melanocytic nevi exceed 1 cm in size, especially when such lesions occur on the trunk. Depending on their location on the skin, they are classified as below:
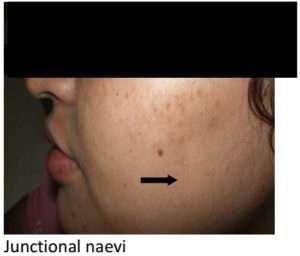
- Junctional melanocytic nevi are generally macular and typically range from brown to brownish-black.
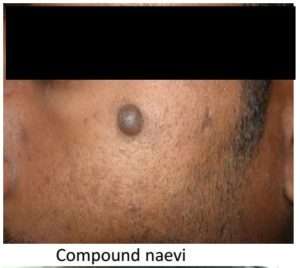
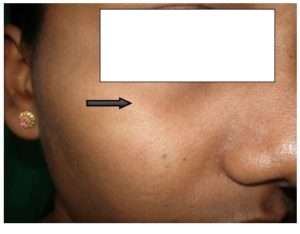
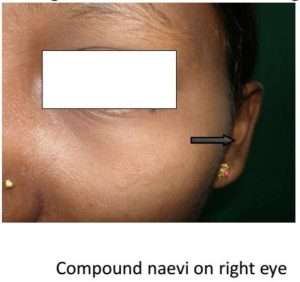
- Compound naevi are benign proliferations of melanocytes in the epidermis, showing evidence of migration of cells into the dermis and ‘maturation’ of those cells within the deeper dermis. Hence they have both epidermal and dermal components.
- Intradermal naeviare benign tumours of melanocytes in which there is no longer epidermal proliferation; the naevus cells have migrated into the dermis and mature there. They are generally skin coloured lesions. Compound and Intradermal melanocytic naevi display elevation relative to surrounding uninvolved skin and hence present as papules or nodules.
Management
Treatment for acquired melanocytic naevi is usually sought for two reasons:
- Diagnostic purpose to rule out malignancy
- Therapeutic purpose for improving aesthetic appearance
The development of a new area of pigmentation within a long-standing non-pigmented or lightly pigmented compound or Intradermal melanocytic nevus is a cause for concern. While pigmentary changes could be due to incidental inflammation or recent irritation or trauma, the possibility of evolving melanoma cannot be ignored.
Investigations:-
The patient has to be subjected to routine blood tests and histopathological evaluation as follows and send the excised specimen for histopathological examination to rule out malignancy:
- Complete blood count, platelet count BT, CT
- Blood sugar
- Serum Creatinine
- VDRL
- Hbs Ag
- HIV
Pre-Procedure Counseling:
- Patient has to be properly counseled and explained This helps in better compliance and a better patient doctor rapport and lesser medico-legal issues for the operating doctor.
- Pre-operative photographs and an informed consent form duly signed by the patient forms an integral part of the pre-op preparation.
- Physical fitness of the patient should be assessed, if a known case of diabetes or hypertension, necessary precautions should be taken.
- If on any medications like NSAID or aspirin, it should be discontinued for 2 weeks before the date of procedure.
Procedure:-
Local anesthetic is infiltrated around the naevi. Plain lignocaine or with adrenaline is used accordingly.
Topical EMLA cream can also be used in cases of Junctional naevus. Once the area is anesthetized, cleansing and scrubbing is done and draped.
ELLIPTICAL EXCISION:-
Here, the naevi is excised from the skin in an elliptical manner keeping the incision aligned along the RSTL and later this is sutured in bi-layered manner to achieved better cosmesis. This method has various advantages and is preferred when the naevi has to be subjected for biopsy in suspected cases of malignancy.
Procedure:
- Instruments required: Surgical bard parker no 15, Adson’s forceps, skin hook, undermining scissors, surgical marker, needle holder, sutures including both intradermal and skin, sizes of which differ according to the area of the skin being operated upon. Usually prolene and vicryl is preferred.
- With a surgical marker the naevi is marked, taking care to align it along the resting skin tension line.
- With a surgical blade no 15 incision is made along the marked region, cross hatching is avoided.
- With a toothed forceps the edge is lifted and skin with the naevi is excised with the surgical blade.
- The edges are undermined with an undermining scissors.
- Intradermal sutures are put with absorbable sutures
- Skin closure is achieved with non absorbable sutures.
Advantages: –
- Surrounding normal skin can also be subjected for biopsy
- Depth of the lesion can be controlled
- Suitable for detecting suspected cases of malignancy
- Aesthetically better result since lesion excised along RSTL
- Excision aids in both therapeutic and diagnostic applications
Disadvantages:-
- Surgical skill needed, since it involves suturing
- Chances of recurrence if malignant lesion is not excised completely
- Small to medium sized moles can be removed and sutured, larger area, if excised requires skin graft for closure.
Indications: –
- Diagnostic purpose: To rule out malignancy
- Therapeutic purpose: Excision of naevi which are suspicious and for aesthetic purposes.
Contraindications: –
- Active infection, keloidal tendency, bleeding diathesis, diabetes.
- Lesions around important structures like eyes and mouth, joints etc should be avoided since it results in contractures
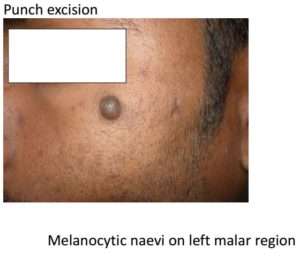
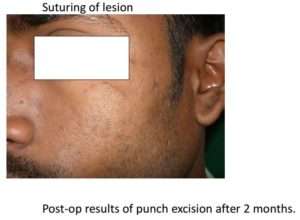
PUNCH EXCISION:
This technique is performed with the help of a metallic cylindrical punch with sharp edges. The punches are selected depending upon the size of the lesion and are available from 1 mm to 5 mm sizes.
Instruments: – disposable or autoclaved punches, skin hooks, undermining scissors, skin sutures.
Procedure:
- A disposable punch is selected according to the size of the naevi.
- Skin is stretched between the index finger and thumb.
- Punch is driven around the lesion and turned in clockwise direction.
- Rotation of the punch is stopped when there is a feel of giving away.
- The naevi, included in the punched out area will appear to float in the surrounding skin.
- Punched out lesion is lifted with a needle and the base is cut from the surrounding skin with scissors.
- Hemostasis is achieved if the size of naevi is small and skin is left to heal by secondary intention.
- If the lesion is larger, skin closure is achieved by using non-absorbable sutures.
Advantages:-
- Easy to use since it requires less skills.
- Requires lesser time.
Disadvantages:-
- May result in dog-ear during repair of the circular defect on skin.
- Blind procedure, hence depth of the lesion excised cannot be controlled, resulting in recurrences.
- In suspected cases of malignancy, perilesional skin is not available for histopathological evaluation.
Indications:-
- Elevated naevi
- Useful in lesions involving subcutaneous tissue.
Contraindications:-
- Active infection, keloidal tendency, bleeding diathesis, diabetes.
- Suspected cases of malignancy.
- Friable and fragile tissue
SHAVE EXCISION
A technique where in the elevated lesion is shaved from the skin using either a surgical blade or sterilized razor blade. The depth of the lesion removed can be controlled leaving the dermis intact hence resulting in minimal scarring.
Instruments: – Sterilized razor blade or no 15 bard-parker surgical blade.
Procedure:
- The lesion to be excised is held and stabilized with the index and thumb finger of the left hand.
- The blade is held with the right hand parallel to the surface of the lesion.
- With a to and fro movement maintained along the base of the lesion, it is sawed in-toto and separated from the base.
- The lesion is released from its base and remains on the blade, thus any remaining attachment is cut with the help of scissors.
Advantages:-
- Easy to perform, lesser skills required.
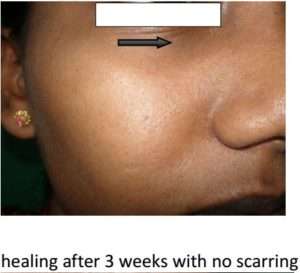
- Scarring is lesser since the dermis is left intact resulting in good aesthetic results.
Disadvantages:-
- Cannot perform in cases of suspected malignancy.
- Difficult to perform if lesion is not intact.
- If the depth is more may result in scarring.
Indications:-
- Lesions on concave areas of body surface.
- Elevated naevi.
- Excisions where aesthetic outcome is a priority.
Contraindications:-
- Active infection, keloidal tendency, bleeding diathesis, diabetes.
- When malignancy is suspected.
- Flat lesions.
RADIOSURGERY:-
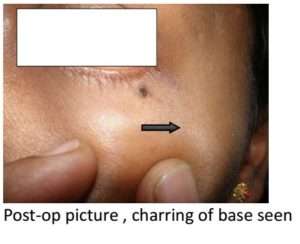
Commonly performed office procedure for excision of lesions, based on thermal ablation and destruction of tissue with a frequency of alternating current in the range of radiowaves. To perform the procedure a radio surgical unit with tungsten electrodes is required. With this unit, cutting of the target tissue, excision along with control of blood loss through homeostasis is achieved.
Procedure:-
- The electrode is selected according to the target tissue and power intensity is adjusted .Target tissue is marked and the electrode angled perpendicular to the lesion and incision is made along the margins of the lesion.
- With an Adson’s forceps the tissue is grasped and the electrode is forwarded beneath the tissue in case of a small lesion. Flat lesions are approached form above downwards.
- The tissue is excised and the remnants are carefully removed, taking care to differentiate between naevus tissue and charred normal skin.
- Homeostasis is achieved by pressure or using the option of coagulation.
- Depth of the lesion removed should be controlled since it may result in scarring.
Advantages:-
- Easy to perform , office procedure
- Less time consuming,
- Lesser tissue damage, thus resulting in fewer complications.
- Better option for excision of lesions on thinner skin like eyelids.
Disadvantages
- Larger lesions may result in scarring
- Cannot be used in cardiac patients.
- Recurrences occur if not excised adequately.
- Pigmentary disturbances post procedure may occur.
Indications:-
- Flat lesions and small elevated lesions.
- Lesions around the structures of the face like – eyes, mouth and nose.
Contraindications:-
Active infection, keloidal tendency, bleeding diathesis, diabetes
- Patients suffering from cardiac disease, with pacemakers, metallic prosthesis.
- Use of spirit or alcohol based cleansers.
LASER SURGERY:-
Ablative lasers such as Co2 and Erbium: Yag have been used successfully for surgical removal of moles. Though not used very commonly, laser surgery is preferred since it can be used in cardiac patients and is less painful, provides an almost bloodless field since there is coagulation of blood vessels. Local anesthesia is avoided hence all the side –effects and complications associated with local anesthetic.
The cost of these procedures along with the chances of post-inflammatory pigment disturbances are the disadvantages with this procedure.
Conclusion:-
Naevi are common skin conditions which usually do not warrant any treatment. However, in some tradition, presence of naevi in certain sites is regarded as inauspicious. Many patients seek treatment to overcome this superstition. Seeking treatment for cosmetic purposes is also on the rise. At present, there is choice of various modalities of treatment available, and it is the duty of a dermatosurgeon to provide the best possible option to a patient. With proper selection the right procedure, good cosmetic results can be achieved.
The authors have tried various modalities of treatment for mole removal and opine that excision and suturing along RSTL is the best option available as it offers good cosmetic results. However the choice of a procedure may be discussed with the patient and decided as per the patients needs.
A recent study conducted by the King’s college of London states that in a case, a series of patients with more than 100 moles had lesser instances of osteoporosis and fewer wrinkles. So the day may not be far away when cases of mole removal for cosmetic reasons may actually decline and moles may be perceived as good omen!

![]()



![]()



![]()




*-*-*