Current concept on structure and function of stratum corneum
Currently, it is considered that over 90% of the skin barrier function resides in the epidermis and particularly in its outermost corneous layer (stratum corneum). The morphological structures, constituting the skin barrier develop relatively late in the ontogenesis (about 34th gestational week). The skin barrier is not fully competent immediately after birth and develop in the earliest stages of the neonatal period.3,4
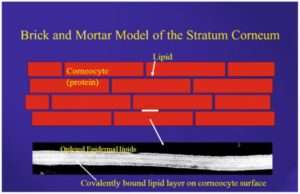
Earlier it was considered that stratum corneum (SC) was an inert layer of dead cells formed in the keratopoesis, interconnected through intercellular lipid layer.5 In recent decades, the SC is viewed as layer of protein enriched corneocytes embedded in lipid-enriched, intercellular matrix, the so called “bricks and mortar’ model.
The bricks are the corneocytes surrounded by a cornified envelope made up of proteins, and covalently bound to the hidroxyceramide molecules of a lipid envelop. In turn, there bricks are embedded in a mortar of lipid bilayers. The so called mortar consists of a variety of intercellular lipid including 50% ceramides, 25% cholesterol and cholesterol esters, 15% free fatty acids and other lipid presented in small concentrations.6
Stratum corneum lipids and biosynthesis of ceramides
The lipids of the SC are substantially different from those constituting other biological membranes in the body. Ceramides structurally a heterogeneous family of lipids that contain long main hydrocarbon chain omega-hydroxy acid and 6-hydroxysphingosine as a binder.
Human SC contains 12 free extractable ceramides fractions with different hydroxylation pattern in sphingoid base and in the fatty acid (FA) moiety. Ceramides have been classified based on their chromatographic migration (ceramides 1-8) or based on the chronology of publications (ceramides 9 onwards) or based on molecular structure (such as sphongosine, sphinganine, 6-hydroxy sphinogosine etc.)
The three main classes of SC lipids are derived from their precursors – phospholipids glycoceramides, sphingomyelin and unbounded sterols are synthesized within epidermis only.
The most important sphingolipids of keratinocytes are glucocylceramides (GlcCers) and ceramides containing a board range of FA species.
They form a template on the surface of corneocytes to organize the extracellular lipid layers as a barrier in the interstices of the SC. Ceramides with ULC-FAs (Ultra long chain – FAs) are major components of the barrier, the extracellular multilamellar lipid layer of the SC, but not of cellular membranes.
Pathological skin disorders
A number of skin pathologies directly cause structural alterations in the SC resulting in the loss of barrier function. In this respect, the most cited skin pathologies are psoriasis, atopics dermatitis, some form of ichthyosis and severe xerosis.
Xerosis, Atopy and Lipids: Epidermal Lipid Status
Dry skin is characterized as a deficiency in stratum corneum ceramides, often correlated to an impaired barrier function. Deficiencies are mostly observed in 6-OH-4-sphingonine and phytosphingosin containing ceramides, which are in majority in human stratum corneum.
In dry skin, the total bound ceramides are deficient of about 30%. All major classes of bound ceramides (CER A;B and Phyto) show identical deficiency and more specifically CER B.
Atopic dermatitis, which is one of most common form of chronic eczema, is characterized by dry skin high frequency of bacterial infection, hyper-responsiveness to environmental stimuli and increased incidence of irritant contact dermatitis.
In atopic dermatitis be accompanied by alternations in the epidermal barrier function including reduced water content and an augmentation in transepidermal water loss (TEWL).
Ceramides have been shown to reduce in atopic dermatitis and ceramides metabolism abnormalities are through to be etiological factor for dry and barrier disrupted skin.
Ichthyosis
Ichthyosis comprises a wide group of inherited and acquired ‘retention hyperkeratosis’ characterized by thickened and scaly stratum corneum. Although the stratum corneum lipid profiles in ichthyosis patients have not been fully determined, reduced levels of sphingosine have been found in these patients.
Psoriasis
Psoriasis is a hyper proliferative disease of the epidermis characterized by abnormal epidermal maturation leading to an incomplete process of differentiation with a consequently defective skin barrier function.
These morphological findings are consistent with the biochemical studies that show a decrease in relative free fatty acid content and a different pattern in ceramide distribution in psoriatic plaques compared with normal control skin. In psoriatic skin, the phytosphingosine-carrying ceramides Cer 3 (NP) and cer 7 (AP) show a statistically significant decrease versus normal stratum corneum.
Dietary Glyceryl ceramides and epidermal lipid barrier
Delivering ceramides to epidermis through oral route is emerging as promising therapeutic option. Evidence is being accumulated depicting the probable mode of action and possible therapeutic benefits beside reducing the TEWL.
Improvement in lipid content
Studies conducted on orel GlcCer have shown that orally administrated GlcCer is absorbed in lymphatic circulation. Radiolabelled study reported on ceramides, notes that after oral consumption of ceramides the sphingoid base could reach epidermis within 24 hrs. Various reports show that oral GlcCer can help boost barrier function by increasing lipid contents in the epidermis.
Effect on tight junctions
1 Tight junctions present in the granular layer are important for barrier function as they control paracellular permeability. TJ components include claudin, occluding, and junction adhesion molecules (JAMs) and junction proteins zolula occludent-1.
2 Sphinogisine and phytosphingsine metabolites of GlcCer have shown to increase the expression of claudin-1 in mice model. Increase in the claudin-1 expression may be directly linked to the recovery of the tight junctions which are compromised in AD or with exposure to UV radiation.
Conclusion
Overwhelming evidence is available depicting role of compromised skin barrier in pathogenesis of inflammatory skin conditions. Promising evidence exists showing potential benefits offered by oral GlcCer such as HLE inhibition, improvement in tight junctions and increased expression of ceramides synthase. However, more studies are required to further substantiate the clinical efficacy of oral GlcCers.






