Any doctor passing out of his alma mater, be it the MBBS, MS or MD/ DVD, the general impression is that once the university grants a degree and there is reasonable amount of confidence, he or she is ready for private practice. Having found a rented space or own premises, the neo-dermatologist is ready to test his skills at treating patients on his own! The volume of practice any physician develops in the first few years is directly proportional to the ability to retain patients. It would be wise to remember that in dermatology, this is all the more important.
Understand one’s speciality:
Every physician needs to essentially understand the limitations of his/her speciality. One cannot forget that dermatology as a specialty deals predominantly with disorders which are chronic, recurrent and sometimes incurable. As a result the patient has to keep revisiting the dermatologist several times to get a reasonable degree of improvement.
Besides, many conditions are related to the environment or lifestyle which cannot be altered greatly. For example, a vegetable vendor who is suffering from a photosensitive disorder cannot maintain sun-protection all the time due to which the dermatosis is bound to recur. In such a scenario, the frustration of the patient rises with each follow up visit which may lead to loss of faith in the doctor, although it is not his doctor’s fault! Therefore, it is very important to develop a strong bond with the patient so that he/she feels that you are genuinely trying to help him/her.
![]()
Strength of bond:
It is well known that at any time of the day outside some physician/specialist’s consulting rooms, there is always a huge crowd of people. Some of them seem to be waiting for several hours without feeling distressed although they would be eager to reach home early. What holds these people back from visiting another doctor who can see them without so much waiting? It is the bond that these patient develops with their doctor, so the wait is worth the while. Based on opinions from several senior practitioners, here are some simple tips to build a great professional relationship with your patients:
Lend a patient ear! :
When a new patient comes for consultation, he is eager to explain everything about his illness from day one. He may go into a lot of unnecessary details about treatment and investigations. If the doctor has a large crowd waiting or he is in a hurry to leave for a dinner party, he may want to cut short the patient’s ramkahaani!
Please beware! The first consultation lays the groundwork for a long-term relationship.
Irrespective of the schedule of the physician, the patient should be given an unhurried hearing. Once the patient develops faith in the doctor, the further consultation with him will become easier and shorter. Listening is an important part of medical consultation, please remember.
Examine minutely:
It is an obvious fact that in most cases, dermatologists can diagnose the disorder and prescribe drugs even before the patient takes his seat in front of the doctor. Yet, allow few seconds to look at the lesion and trying to gauge what the patient feels before scribbling into the prescription pad.
Holding the magnifying glass on each lesion for some time could be a waste of time for the dermatologist but for the patient it appears as if the doctor is thinking and analyzing the lesion. Every dermatologist can treat dandruff by simply hearing the complaint. However, actually palpating the scalp and nodding to the patient that the scaling is indeed troublesome, does a lot for human relationship.
Check irrelevant reports too:
Very often patients who are not too knowledgeable about medical matters bring a big pile of blood reports, X-rays etc. In most cases, although these reports are of no clinical value to the dermatologist it would be a good idea to patiently take a look at them when the patient shows it, regardless of the rush. This would give an idea to the patient that the doctor appears to be alert to the patient’s problem.
If one was to brush it off casually without checking any report, the patient may be offended as he would have spent a lot of time and money to get these tests done. The entire exercise goes a long way in building an emotional bond with the patient.
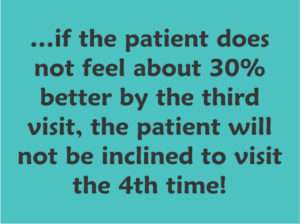
3rd visit smile:
Everyone knows that skin disorders can take a long time to get better. Yet if the patient does not feel about 30% better by the third visit, the patient will not be inclined to visit the 4th time! While every dermatologist tries to make the patient happy, it is important that the time frame for improvement is kept in mind. As time passes, the patient’s patience wears off and with it, his faith in the doctor reduces. Once some recovery is seen on the third visit, most patients would give more time for further recovery, extending the hope-line!
Explain, explain:
For intelligent patients, elaborate on the disease and its progression in the first visit. Quite often he has searched internet and is ready with a lot of information. In recurrent diseases, indicate that there are drugs like retinoids, immune-modulators and biologics available but explain that you would reserve the tougher drugs only for difficult lesions!
Educated people can be taken into confidence while prescribing drugs so that their accurate feedback helps both parties. This also helps to seal the patient-doctor relationship, making the difficult period for the patient less stressful and also helps the dermatologist think freely without having to show magical results instantly.
Clarify prescription:
Every physician is expected to write prescriptions legibly. In India handwritten prescriptions are sometimes pathetic to read and even the chemist barely guesses the scrawl and manages to dispense drugs. Let others do what they wish, but the young dermatologist should make a good beginning with neat hand-writing. Not only should it written clearly, but also explain each medicine to the patient with the dosages etc.
Be specific about when to take the tablets/syrup with reference to meal times. Patients need to be specifically explained about when to apply creams i.e. after bath, bedtime or so many minutes before sun exposure. This small extra effort in interacting with the patient will not be easily forgotten, please note. It will also ensure fewer telephonic calls saying, “doctor, you did not tell me when to apply Perlice cream.”
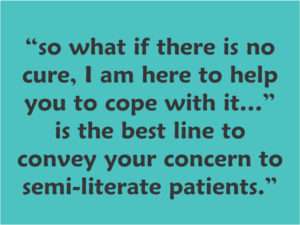
Be willing to stand by:
Understand the level of intelligence of the patient. If he is not literate, do not go into technical detail, but indicate by your warmth, that you are there to help him always. Note that by providing more information that the person can handle may scare the unschooled or illiterate to think that there is something dangerous happening to him. For such people, “so what if there is no cure, I am here to help you to cope with it…” is the best line to convey your concern.
In conditions like psoriasis, relapses are depressing and it is at times like these that empathy helps. Assure him/her that we can find a way to give some relief.
Pause, ponder
All these points may seem trivial at first, but when one pauses to understand its real meaning we can put most of them to practical use. As one becomes senior in the profession, most of these suggestions will come into play automatically without any extra effort, provided they have been implemented into our work-system time and again.
Many years later, there will be a smile on your lips when a patient who had consulted you say 5-years ago returns to you with a new complaint, saying “Doc, I have got transferred to another town but when I developed this skin rash, I could only think of coming to you!”






