What is Nanotechnology?
Nanotechnology can be described as a collection of methods and techniques for processing materials at an atomic and molecular scale to create products with special physicochemical properties such as rigidity, hydrophobicity, size, shape, charge, conductance, chemical reactivity, magnetism in relation to conventional products. It deals with materials less than 100 nm. There are two major approaches to get the nano particles -one is the bottom up and the other is top down approach. Top-down fabrication reduces large pieces of materials all the way down to the nano scale while bottom-up approach to nano manufacturing creates products by building them up from atomic- and molecular-scale components.
History of Nanotechnology:
The idea and concept behind nanotechnology started with a talk entitled “There’s Plenty of Room at the Bottom” by physicist Richard Feynman at an American Physical Society meeting at the California Institute of Technology (CalTech) on December 29, 1959, long before the term nanotechnology was used. Feynman described a process in which scientists would be able to manipulate and control individual atoms and molecules. Over a decade later, Professor Norio Taniguchi coined the term nanotechnology, in his explorations of ultraprecision machining. In 1981, with development of the scanning tunneling microscope that could see individual atoms by IBM and the modern nanotechnology era began.
Type of Nanoparticles:
Nanoparticles fall into 3 categories:
1) Naturally occurring: particles constantly present in nature such as ashes produced from volcanoes, dust, nanoparticles produced from water bodies and plants, viruses etc.
2) Incidental: It includes combustion products, industrial processes, vehicle emission, from construction process, welding fumes etc.
3) Engineered: They are formed for human welfare and divided into organic and inorganic.
Organic particles namely lipososmes, dendrimers, fullerenes, PAMAMS, ISCOMS, polymerised particles, solid lipid nanoparticles, nanostructured lipid carriers.
Liposomes:
Liposomes are biocompatible, versatile and have good entrapment efficiency. It finds application as long circulatory delivery of gene, drug, protein and peptide.
Fullerenes:
They are 1-nm carbon spheres of 60 carbon atoms and capable of carrying genes, proteins and other biomolecules for delivery purposes.
Dendrimers:
They are hyper branched, tree-like structures. Unimolecuar structure with size of 20nm & used to transport medication.
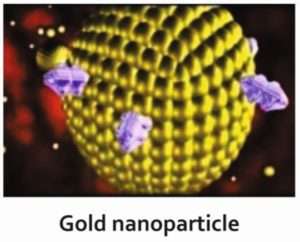
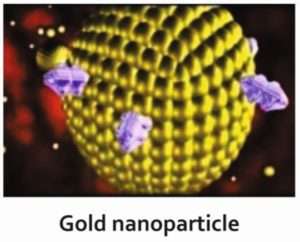
Inorganic nanoparticles are made of metal (gold or silver), metal oxide (iron), and ceramic material (silica), encapsulating medication in their interior, transferring and liberation various substances, quantum dots and carbon tubes.
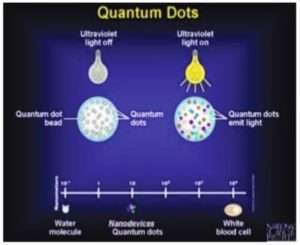
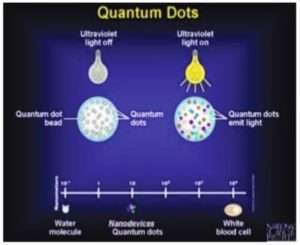
Quantum Dots are 2-10nm nanocrystalline semiconductor material made from cadmium selenide with an exclusive spectroscopy and with optical properties good candidates for diagnostic applications.
Carbon nano tubes: These are unique for their size, shape, and have unique physical properties. Nano tubes have some special advantages over other drug delivery and diagnostic systems due to their unique physical properties.
Applications of Nanotechnology in Dermatology:
Broadly classified into 3 categories:
- Cosmeceuticals: sunscreens, volatile compounds like insect repellents, perfumes, emollients, anti-wrinkle creams.
- Diagnostic devices: Carbon nanotubes, Quantum dots, Nanopunches
- Therapeutic devices:As drug delivery carriers, or nanosized drug itself.
1) Cosmeceuticals
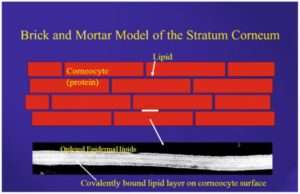
Nanoparticles are used to encapsulate a vast range of substances beneficial to skin. In this way nanovesicles are developed for both pharmaceutical and cosmetic use. They are applied over the skin and these agents enter either through the upper layer of skin known as stratum corneum or through the hair follicles.
Sunscreens are one of the most commonly used over-the-counter drugs. Nanoparticles of titanium dioxide and zinc oxide are used in sunscreens which increases the efficacy, decreasing the white effect remain after using the conventional ones and decreases their stickiness and covering the skin more evenly. While use of nanoparticles in moisturisers increases their permeability into skin.
Use of botulin toxin and hyaluronic acid used as anti-ageing agents. Hyaluronic acid in its bulk form is 50,000 nm or larger in size and is unable to penetrate skin when applied topically. While nanosized particles of hyaluronic acid can penetrate the skin and are the basis of a topical delivery system in development. Botulinum toxin has been stabilized and encapsulated in a form that allows penetration of the skin and apparent effacement of rhytides in early clinical trials.
Chitin nanofibrils are natural polysaccharide obtained from crustacean shells after carbonate and protein removal. These nanofibrils activate keratinocyte and fibroblast proliferation, cells present in skin, and regulate collagen synthesis.
Other uses like slow release kinetics are important for perfumes, which can yield all-day fragrance. They are also useful for insect repellents, such as N, N-Diethyl-meta-toluamide (DEET), to prolong efficacy. Nano-emulsions provide a new colloidal drug delivery system that efficiently replaces lost lipid in epidermis.
2) Therapeutic:
A) As a drug delivery system:
Used as carrier for different drugs with benefits of site specific drug delivery, lesser side effects, more duration of action of the drug due to sustained release, protecting the therapeutic agent from chemical, physical and biological damage and increased cellular uptake of drug.
Thus variety of nanoparticles such as dendrimers, lipososmes, polymeric nanoparticles, solid nanoparticles, nano structured lipid particles etc are being used as drug delivery system. They encapsulate the drug and deliver it to the desired site.
Drugs which are commonly used nowadays with nanotechnology are analgesics with their sustained release properties, antibiotics covered with polymeric nano particles, cortico-steroids decreasing inflammatory process inside the body, drugs for hair fall, acne treatment, anti-fungals, silver used as an anti bacterial agent in wound dressing and many agents are being used in many other diseases.
Antisepsis is another big area for nanoparticle operation. Chlorhexidine gluconate carried by nanoparticles (Nanochlorex®) is having an immediate antibacterial effect. The most commercialised antibacterial nanomaterial to date is nanosilver, used not just in wound and burn dressings but also as water disinfectant and room spray.
B) In treatment of malignancies:
Due to the small size of nano particles can be of great use in oncology, both in diagnosing and treating malignancies. Nano shells coated with gold were used to kill cancer tumors in mice by Prof. Jennifer at Rice University. These nano shells are targeted to bond to cancerous cells by conjugating antibodies or peptides to the nano shell surface. Area of the tumor is irradiated with an infrared laser, which heats the gold sufficiently and kills the cancer cells.
Nanoparticles are used in cancer photodynamic therapy, wherein the particle is inserted within the tumor in the body and is illuminated with photo light from the outside. The particle absorbs light and if it is of metal, it will get heated due to energy from the light. High energy oxygen molecules are produced due to light which chemically react with and destroy tumors cell, without reacting with other body cells. Photodynamic therapy has gained importance as a non-invasive technique for dealing with tumors.
C) Gene Silencers:
Gene silencing is currently one of the most promising new approaches for disease therapy. This is useful in genetically inherited diseases or diseases occurring due to mutation in genes. Small interfering RNA (siRNA) showed significant potential in new molecular approaches to down-regulate specific gene expression in mammalian cells. However, RNAs cannot easily penetrate cell membranes; therefore RNA delivery becomes one of the major challenges for gene silencing technology. Small interfering ribonucleic acids encapsulated with polymeric nanoparticles can precisely inactivate the gene expression and hence useful in genetic disorders.
3) Nano-diagnosis:
One of the important uses of nanotechnology is directed towards development of improved diagnostic techniques to screen complex diseases. Screening indicates identification of the cause of illnesses, monitoring the improvement or progression of the state of diseases such as cancer, cardiovascular or neurodegenerative diseases.
Nanotechnology enables the manipulation of materials at nanoscale and has shown potential to enhance sensitivity, selectivity and lower the cost of diagnosis. Several types of nanomaterials such as metals, metal-oxides and quantum dots have shown ample advantages over traditional diagnosis.
Quantum dots, with quantum confinement properties, can be used in conjunction with MRI, to produce exceptional images of tumor sites. Fluorescent quantum dots produce a higher contrast image and at a lower cost than organic dyes used as contrast media. It works on the principle of absorbing light of desired wavelength and having envelope with fluorescence signal. When tagged with antibodies they emit fluorescence that helps in diagnosing tumours
In malignant melanoma, topical application of quantum dots will allow sentinel lymph node evaluation without disturbing the skin and used as a non-invasive method to evaluate the spread of malignancy.
Gold nanoparticles, in combination with fluorescent protein, are being used in diagnosis of cancer by emitting fluorescence when binding occur with the target atypical cell.
Carbon nanotubes 0.5–3 nm in diameter, are specialised structures having good conductivity with special property of alteration in their conductivity on binding to macromolecules like nucleic acids and antibodies, their conductivity changes. They are used in diagnosis of skin infection and malignancies, for detection of DNA mutation.
Nanopunches are small simple biopsy tool that is made from silicon, chromium, nickel & copper. Having unique shape of ‘órigami claw’ like, its movement and excretion controlled by magnetic field and useful to obtain biopsy from difficult sites like nail matrix, fascia, liver etc.
Iron oxide nanoparticles can used to improve MRI images. The magnetic property of iron oxide enhances the images from the Magnetic Resonance Imagining scan.
Adverse Effects:
1) Formation of foreign body granuloma
2) Scleromyxedema i.e hardening of organs
3) During pregnancy can be hazardous for the foetus
4) Free radical injury to the cells by particles TiO2
5) Act as hapten or cross reactant and can start allergic reactions
Nanoparticles are present in our atmosphere since the origin of earth, for example as the result of combustion processes (forest fires), in volcanic ash, or as dust in the air due to weathering and erosion. In the modern era, they are unintentionally produced due to human activities like household heating, industry, slash-and-burn clearance, transport. All these things adversely affect the atmosphere and the creatures but no studies are available that can explain the mechanisms of uptake, distribution, metabolization and excretion of nanoparticles and exact damage they are causing to environment.
Advantages of Using Nanotechnology:
1) Increases efficacy of drugs
2) Provides a site specific drug delivery therefore reducing uneventful side effects
3) In cosmetology, having many indications and used in anti-ageing process
4) It improves the diagnosis and treatment of many diseases
5) As a gene therapy can prevent the inherited diseases
6) Nano-built devices can be implanted in body to continuously adjust body’s chemical balance
There is a never ending list of benefits delivered by nanotechnology in different fields apart from health and medicine. It gives a new way of providing healthcare to humans.
References:
Nasir A : Nanotechnology and dermatology: part 1 –potential of nanotechnlogy. Clin Dermatol. 2010;28(4) : 458 -66
Ali R , Hussain I –Nanoderamtology : new horizon . J Pak Assoc Dermatol.2013;23(2):117-9
Newman MD, Scotland M , Elis JI . The safety of nanosized particles in titanium dioxide and zinc oxide based sunscreens . J Am Acad Dermatol. 2009;61 (4):685-92.
Nanodermatology society. Available from: http ://www.nanodermsociety.org/index.php.